Molar Pregnancy - H Mole Or Hydatidiform Mole
Complications
Obie Editorial Team
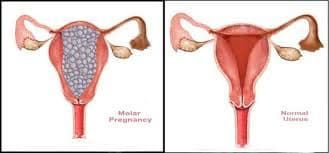
A molar pregnancy occurs when the placenta develops into an abnormal mass of cysts rather than becoming a viable pregnancy.
Molar pregnancy is a type of gestational trophoblastic disease (GTD). In a complete molar pregnancy, there's no embryo or normal placental tissue. In a partial molar pregnancy, there's an abnormal embryo and possibly some normal placental tissue. The embryo begins to develop but is malformed and can't survive.
A molar pregnancy can have serious complications — including a rare form of cancer — and requires early treatment. Careful monitoring after a molar pregnancy can help preserve the chance for future healthy pregnancies.
A molar pregnancy can have the following symptoms:
- Rapid growth of the uterus
- Uterus bigger than dates (though many can be thge same size or even smaller)
- Normal first trimester symptoms or persistent nausea and vomiting
- Bleeding or spotting in the first or second trimester. ( spotting or heavy, intermittent or continuous, usually light)
- No fetal heart tones or fetal movement
- Pelvic pressure
- Hypertension may become a problem in the second trimester
- Shortness of breath (late, life threatening indication of an embolism)
- Enlarged, tender ovaries (ovarian cysts)
- Passage of "grape-like" vesicles with bleeding
The diagnosis of a molar pregnancy is made by ultrasound and by elevated beta hCG levels. There is a rare risk (two percent) of choriocarcinoma (cancer) following molar pregnancy. Benign tumor formation may also occur.
Treatment involves evacuation, usually with suction curettage, of the vesicles within the uterus. Lab studies might include serial beta hCG levels, blood clotting studies, liver and thyroid profiles, hemoglobin, and chest X-ray.
Beta hCG levels are drawn every one to two weeks until resolved and then they may be done on a regular schedule for the year following the loss.
Because the risk of cancer needs to be fully evaluated, effective contraception should be used for one year following the pregnancy. Regular visits for a physical and pelvic exams are made until the uterus and ovaries are back to normal. Thereafter, they are generally done every three months for the next year.
In subsequent pregnancies, the woman may be at higher risk of another molar pregnancy, so she is followed closely with serial hCG levels and ultrasound.