Where To Start If You Are Having Trouble Getting Pregnant
Infertility
Obie Editorial Team

It takes on average 4-6 months to get pregnant. If pregnancy does not happen as expected, or there are issues, both male and female fertility testing needs to be done to get tested for fertility.
The first step: Semen analysis
In 50% of couples with fertility issues, there is a male problem, meaning that his sperm evaluation is not normal. Thus, the very first test to do is a sperm count (a.k.a. semen analysis). Only if this test is completed and the results are normal should the female partner undergo further fertility testing.
Medical history and physical examination
The first step in a female infertility workup is a complete medical history and physical examination and the following is reviewed:
- Menstrual history
- Medical history
- Sexual technique and timing
- Lifestyle issues (such as smoking and drug, alcohol, and caffeine consumption)
- Medications being taken
The following steps are free or low-cost and can be helpful:
- Monitor basal body temperature. This is accurate in determining if ovulation is actually taking place.
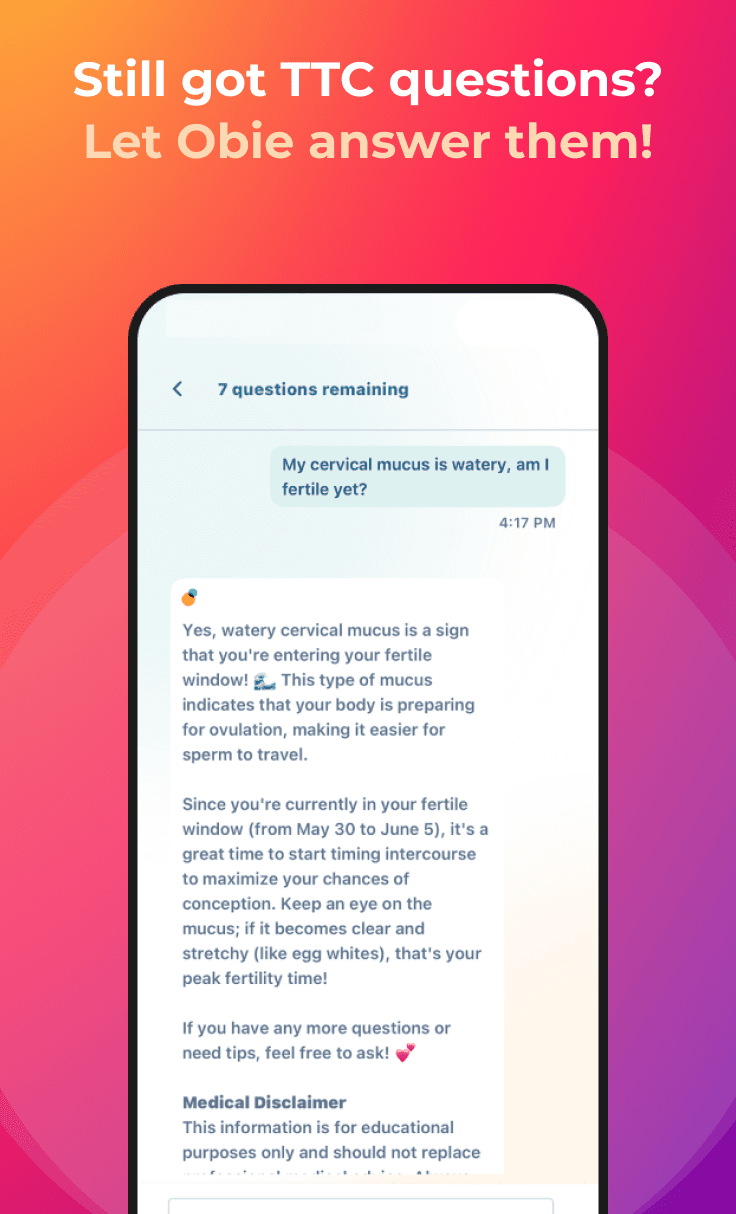
- Test the consistency of your cervical mucus. Collect some mucus between your two fingers and stretch it apart. If you are near the time of ovulation, the mucus will stretch more than 1 inch before it breaks. As an alternative, at-home kits can test saliva as a substitute for checking cervical mucus.
- Take an over-the-counter urine test for detecting luteinizing hormone (LH) surges. This helps determine the day of ovulation.
The next steps consist of several laboratory tests which may be used to detect the cause of infertility and monitor treatments:
Hormone levels
Blood and urine tests are taken to evaluate hormone levels. Hormonal tests for ovarian reserve (the number of follicles and quality of the eggs) are especially important for older women.
Examples of possible results include:
- High follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels and low estrogen levels suggest premature ovarian failure or hypogonadotropic hypogonadism.
- High LH and low FSH may suggest polycystic ovary syndrome or luteal phase defect.
- High FSH and high estrogen levels on the third day of the cycle predict poor success rates in older women trying fertility treatments.
- LH surges indicate ovulation.
Blood tests for prolactin levels and thyroid function are also measured. These are hormones that may indirectly affect fertility.
Clomiphene challenge test
Clomiphene citrate (Clomid, Serophene), a standard fertility drug, may be used to test for ovarian reserve. With the CCCT the clomiphene citrate challenge test, the doctor measures FSH on day 3 of the cycle. The woman takes clomiphene orally on days 5 and 9 of the cycle. The doctor measures FSH on the tenth day. High levels of FSH either on day 3 or day 10 indicate a poor chance for a successful outcome.
Tissue samples
To rule out luteal phase defect, premature ovarian failure, and absence of ovulation, the doctor may take tissue samples of the uterus 1 - 2 days before a period to determine if the corpus luteum is adequately producing progesterone. Tissue samples taken from the cervix may be cultured to rule out infection.
Tests for autoimmune disease
Tests for autoimmune diseases, such as hypothyroidism and diabetes, should be considered in women with recent ovarian failure that is not caused by genetic abnormalities.
Imaging and other procedures
If an initial fertility workup does not reveal abnormalities, as happens in about 40% of cases, more extensive tests will reveal abnormal tubal or uterine findings. The three major approaches for examining the uterus are:
- Ultrasound (particularly a variation called saline-infusion sonohysterography),
- Hysterosalpingography
- Hysteroscopy
- Laparoscopy
Although combinations of these diagnostic approaches are often used to confirm diagnoses, one study indicated that with the introduction of saline-infusion sonohysterography, all are equally accurate and combinations do not increase accuracy. Furthermore, the ultrasound procedure is significantly less painful than the other two, suggesting that this should be the procedure of choice, if available.
Ultrasound and sonohysterography
Ultrasound is the standard imaging technique for evaluating the uterus and ovaries, detecting fibroids, ovarian cysts, and tumors, and also obstructions in the urinary tract. It uses sound waves to produce an image of the organs and entails no risk and very little discomfort.
Transvaginal sonohysterography uses ultrasound along with saline infused into the uterus, which enhances the visualization of the uterus. This technique is proving to be more accurate than standard ultrasound in identifying potential problems. It is currently the gold standard for diagnosing polycystic ovaries.
Magnetic Resonance Imaging. Magnetic resonance imaging (MRI) gives a better image of any fibroids that might be causing bleeding, but it is expensive and not usually necessary.
Hysteroscopy
Hysteroscopy is a procedure that may be used to detect the presence of endometriosis, fibroids, polyps, pelvic scar tissue, and blockage at the ends of the fallopian tubes. Some of these conditions can be corrected during the procedure by cutting away any scar tissue that may be binding organs together or by destroying endometrial implants. (It may miss cases of uterine cancer, however, and is not a substitute for more invasive procedures, such as dilation and curettage ( D&C) or endometrial biopsy if cancer is suspected.)
It is done in the office setting and requires no incisions. The procedure uses a long flexible or rigid tube called a hysteroscope, which is inserted into the vagina and through the cervix to reach the uterus. A fiber optic light source and a tiny camera in the tube allow the doctor to view the cavity. The uterus is filled with saline or carbon dioxide to inflate the cavity and provide better viewing. This frequently causes cramping.
There are small risks of bleeding, infection, and reactions to anesthesia. Many patients experience temporary discomfort in the shoulders after the operation due to residual carbon dioxide that puts pressure on the diaphragm. The wound itself is minimally painful.
Hysterosalpingography
Hysterosalpingography is performed to discover possible blockage in the fallopian tubes and abnormalities in the uterus:
- The doctor inserts a tube into the cervix through which a special dye is injected. (The patient may experience some cramping and discomfort.)
- The dye passes into the uterus and up through the fallopian tubes.
- An x-ray is taken of the dye-filled uterus and tubes.
- If the dye is seen emerging from the end of the tube, no blockage is present. (In some cases, hysterosalpingography may even restore fertility by clearing away tiny tubal blockages).
- If the results show blockage or abnormalities, the test may need to be repeated. In the case of blockage, hysterosalpingography may reveal several conditions, including endometrial polyps, fibroid tumors, or structural abnormalities of the uterus and tubes.
- The test has significant rates of false diagnoses, both positive and negative. There is a small risk of pelvic infection, and antibiotics may be prescribed before the procedure. One study suggested that flushing the tubes with an oil-based fluid (lipiodol) during this procedure may improve fertility rates in women with infertility of unknown causes.
Investigative tests to determine remaining eggs
As women age, the number of follicles (and therefore their egg supply) declines. Researchers are developing tests that may help determine how many are left. Such tests include the following:
- Calculating the volume of the ovaries. In general, the smaller the ovaries, the fewer the remaining eggs.
- Counting antral follicles. Antral follicles are those that develop but do not become dominant follicles. Instead, they form a fluid-filled space called an antrum. Women who have fewer than three to five antral follicles appear to have a poor chance of fertility.
- Measuring inhibin B. Inhibin B is a growth factor produced in the ovaries. Low levels suggest fewer eggs.
Eventually, these markers may be useful for determining which women need more aggressive treatments.
Genetic testing
Genetic testing may be warranted in cases of male infertility or when genetic factors may be causing pregnancy failure in the woman. If genetic abnormalities are suspected in either partner, counseling is recommended.
A technique called preimplantation genetic diagnosis (PGD) is now available in some centers that can examine all the chromosomes in a human embryo. It helps identify abnormalities that increase the risk for infertility, treatment failures, or genetic defects in the offspring.