Coronavirus COVID-19 Pregnancy and Fertility
Infections
Obie Editorial Team

What is COVID? | Symptoms | COVID & Pregnancy | Facts & Myths |
How likely are you now to get pregnant with COVID-19 around us?
For up-to-date accurate medical information on COVID-19, fertility, and pregnancy, go to:
- Resolve
- Society for Maternal-Fetal Medicine (SMFM): Pregnancy and COVID-19
- American College of Obstetricians and Gynecologists (ACOG)
- Centers for Disease Control and Prevention (CDC)
- UpToDate - Pregnancy and COVID-19
- American Society of Reproductive Medicine (ASRM)
- Society for Assisted Reproductive Technology (SART): Coronavirus
- World Health Organization (WHO)
From Johns Hopkins: The most reliable updated count of cases
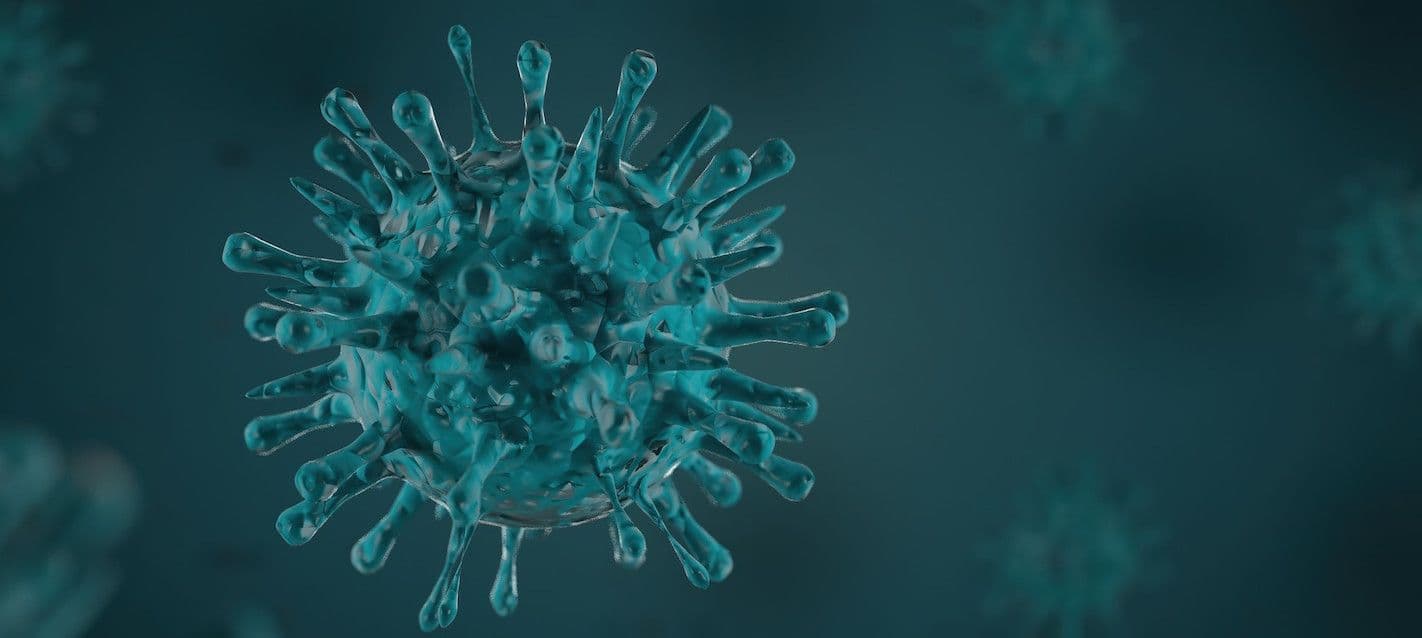
What is COVID-19 (2019-Novel Coronavirus)?
This most recent coronavirus outbreak was reported on January 9, 2020, by the World Health Organization and identified by Chinese authorities. The virus is associated with an outbreak of pneumonia in Wuhan City, Hubei Province, China. On March 11, 2020, the World Health Organization officially named it a pandemic. The flu virus is similar but different. Find out why Coronavirus is not new but this strain is.
What are the symptoms of COVID-19?
Information on the COVID-19 is evolving rapidly. The main symptoms experienced by most people infected with the virus include fever, cough, and shortness of breath. However, some people have reported headaches, body aches, exhaustion, and more. Here is a list of full symptoms and information on how the disease is transmitted.
The New Model of Prenatal Care in the Age of COVID-19
Pregnancy & Coronavirus (COVID-19)
In general, pregnant women can be more susceptible to infections, since pregnancy is a time of low immune function. Based on what we know, pregnant people are not more likely to become infected but they are at an increased risk for severe illness from COVID-19 and death, compared to non-pregnant people. Additionally, pregnant people with COVID-19 might be at increased risk for other adverse outcomes, such as preterm birth (delivering the baby earlier than 37 weeks), miscarriage, and preeclampsia
Drs. Chervenak and Grunebaum recommend that all TTC, pregnant, and breastfeeding/postpartum women be vaccinated for COVID-19.
Here are regularly updated FAQs about COVID-19 from the American College of ObGyn.
More information about COVID-19 and pregnancy:
- Society for Maternal-Fetal Medicine (SMFM)
- American College of Obstetricians and Gynecologists (ACOG)
- Centers for Disease Control and Prevention (CDC)
Data are still in flux and may change daily.
Can the virus be transmitted in the uterus to the fetus?
It is believed that the virus could be transmitted to the fetus before birth. From the few cases that have been reported, it appears newborn babies are not at high risk of becoming infected, but the cases are truly too few to come to any conclusions.
Here are the answers to the most common questions surrounding pregnancy and the Coronavirus.
Male Fertility and COVID-19
The first study to show that COVID-19 infection could potentially affect male fertility was published in November 2020 in the Journal "The World Journal of Men's Health". The study confirmed that the COVID-19 virus was present in the testes of 3/6 patients who dies of coronavirus infection. The authors conclude that "..COVID-19 is prevalent in testes tissue of infected patients.." And they suggest that ".. the male reproductive tract, specifically the testes, may be targets of COVID-19 infection.." This, according to the study suggests a possible mechanism of how COVID-19 can cause infertility in men. Further studies are needed to confirm these findings.
Dispel the COVID-19 myths
Every hour, information on the Coronavirus outbreak changes and everyone seems to have an opinion on what is the best course of action to take to protect yourself, your family, and your community. There are countless “experts” offering their opinions, which are simply not rooted in medical facts and there are also countless people offering completely inaccurate information on social media. In Coronavirus: Separating Fact From Fiction, we break down the medical facts and dispel the inaccurate rumors circulating, such as how long the virus stays on surfaces, whether you get the virus twice, if food delivery safe, and more.
Resources:
- World Health Organization (WHO)
- Centers for Disease Control (CDC)
- What Does the Coronavirus Disease Mean for Families? (From JAMA)
- Cold and Flu During Pregnancy
- What is COVID-19 (2019-Novel Coronavirus)?
- How is Coronavirus Transmitted?
- Thriving During Pregnancy Amid the Coronavirus Outbreak
- Are Pregnant Women at Higher Risk of Contracting Coronavirus?
- Coronavirus: Separating Fact from Fiction
- Is Home Birth Safer During COVID-19
- Treating the Cold and Flu During Pregnancy
- H1N1 Virus
- Infections During Pregnancy
- Real Body Talk: Stop Objecting to Staying Home During COVID-19 Quarantine
Read More